Learning Hub
Explore resources to help you understand and manage psoriatic arthritis.
Psoriatic Arthritis Handbook
Understanding Psoriatic Arthritis
What is psoriatic arthritis?
Psoriatic arthritis is a type of arthritis linked with psoriasis, a chronic skin and nail disease. Psoriasis causes red, scaly rashes and thick, pitted fingernails. Psoriatic arthritis is characterized by joint swelling (inflammation), pain and stiffness and can affect any peripheral joint such as fingers, toes, knees and/or spine. It also affects the insertion of tendons or ligaments in bones (enthesitis).
Between 20-40% of people with the skin condition psoriasis will develop psoriatic arthritis (1, 2). Symptoms affecting their joints tend to develop 5 to 10 years after psoriasis is diagnosed but it can occur at any time (3). Currently, it is not clear why some people with psoriasis develop psoriatic arthritis while others do not.


The arthritis of psoriatic arthritis comes in 3 forms: oligoarticular arthritis that affects 4 or less peripheral joints (e.g., joints in the fingers, toes, knees); polyarticular arthritis that involves 5 or more peripheral joints on both sides of the body; and axial arthritis that affects the joints of the spine including the sacroiliac joint (where the spine connects to the pelvis).
Some people may develop psoriasis after or at the same time as symptoms of psoriatic arthritis present themselves (4). In rare cases, people may have psoriatic arthritis and never have any noticeable symptoms of psoriasis.
Psoriatic arthritis and psoriasis are chronic inflammatory conditions that are caused by a fault in the immune system. Our immune system protects us from infection and illness.
What causes psoriatic arthritis?
While psoriatic arthritis can occur at any age, most people present their first signs and symptoms at 30-50 years. Psoriatic arthritis is most likely to be diagnosed within the first ten years of the psoriasis diagnosis (3).
Psoriatic arthritis affects both sexes equally. However, the manifestations in terms of severity and impact of the disease differ between sexes. Men are more likely to have involvement of the bones in the spine (axial arthritis) and radiographic damage in the spine and peripheral joints (e.g., fingers, knees and toes), whereas women are more likely to experience impaired quality of
life and severe limitations in function (5).
Researchers are not sure why some people develop psoriatic arthritis. It is thought that certain genes inherited from parents and grandparents can make a person more likely to develop psoriatic arthritis (6–8).



In people with a higher genetic predisposition to develop psoriatic arthritis, the condition can be triggered by environmental factors, such as:
-
an infection (9);
-
an accident or injury (10, 11);
-
being overweight (12);
-
smoking (13, 14).
Psoriasis and psoriatic arthritis are not contagious. You cannot catch psoriasis or psoriatic arthritis from other people.
What are the symptoms of psoriatic arthritis?
Psoriatic arthritis symptoms usually develop slowly, that is, many people are unaware that they are developing psoriatic arthritis (Figure 1). Although symptoms can develop suddenly in rarer cases.

Some of the main symptoms include (15):
-
pain in one or more joints;
-
swelling in one or more joints;
-
stiffness in one or more joints that lasts for 30 minutes or longer.
These symptoms are caused by inflammation and can affect any joint in the body. See Figure 2 for the most commonly affected joints.

Psoriatic arthritis can cause pain and swelling in the entheses, that is, places in the body where tendons and ligaments connect to the bones (15). When the entheses become inflamed it is known as enthesitis.
Enthesitis pain can spread along a wider area than joint pain. It frequently occurs at the back of the heel or on the bottom of the foot, which can make standing or walking difficult. Affected areas feel tender to touch even when just a small amount of pressure is applied. The knees, hips, elbows and chest can also be affected by enthesitis.
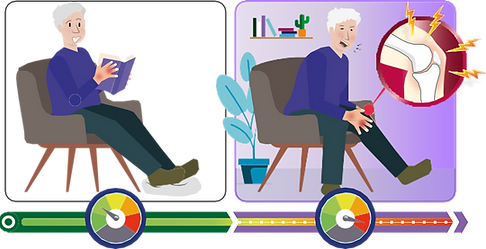
Many people with psoriatic arthritis have swollen fingers or toes, a condition that is known as dactylitis (15) (Figure 1). It most commonly affects one or two fingers or toes at a time.
Psoriatic arthritis can also cause small round dents in fingernails and/or toenails, a condition known as pitting. The nails can change colour, become thicker, or even lift away from your finger (15).
People living with psoriatic arthritis may feel very tired (fatigued) and some may have a low-grade fever. Fatigue does not get better with rest.
Psoriatic arthritis symptoms may come and go. A period of increased inflammation and worsening of other symptoms is called a flare. A flare can last for days or months
How is psoriatic arthritis diagnosed?
A timely and accurate diagnosis is an important step for optimising care and improve long-term health outcomes (16).
If you have been diagnosed with psoriasis in the past, and symptoms of arthritis (e.g., painful or swollen joints) have started more recently, you may have developed psoriatic arthritis. However, the symptoms of psoriatic arthritis can look like other health conditions. Make sure to see your healthcare provider for a diagnosis.
The doctor you see first may depend on whether you have previously been diagnosed with psoriasis. If you develop symptoms of arthritis your primary care or skin doctor should refer you to a rheumatologist – a doctor who specialises in joint conditions – for an assessment.
Tell your doctor if you have a history of psoriasis and/or psoriatic arthritis in your family.
CURRENTLY, NO SINGLE TEST CAN CONFIRM PSORIATIC ARTHRITIS (15).
A diagnosis will be made based on your medical history, symptoms, and a physical examination by your doctor.
Your doctor may order X-rays or other types of imaging, such as ultrasound scans and magnetic resonance imaging (MRI), to look for changes to your bones and joints. Imaging studies will help your doctor determine the type and pattern of joint involvement, which can also help them distinguish between arthritis types.
Blood tests, such as erythrocyte sedimentation rate and C-reactive protein, can help to identify inflammation. Your doctor may also order tests for rheumatoid factor and the anti-CCP antibody to rule out rheumatoid arthritis and HLA-B types to look for your genetic predisposition to
spondylarthritis.
